|
| “Time is Tissue” |
I worked at our respiratory clinic today and saw five patients. I thought it might be interesting to share the process of the decisions that I made, especially in regards to testing.
The first patient tested positive for COVID-19 early this month. He had been doing better and has actually been back to work for a week for a transportation company. In the last week he has felt a lot of his symptoms start to come back. I was frankly more worried for a secondary infection rather than prolonged COVID. A chest X-ray did not show pneumonia. A blood count was ordered. Since he was actively working, I told him to stay at home. I did repeat the COVID test just to make sure he was not still actively shedding virus while being out in the community.
The next patient had mild symptoms. He had a slight cough for nearly two months. He had no other symptoms nor medical issues. He was retired and staying at home so I did not feel that his symptoms warranted testing. The time frame certainly did’t fit for COVID. He was reassured but told to call if he got worse.
Later a husband and wife came in together. He was known to have COVID and had been hospitalized for two days earlier in the month. He felt like he had been improving but like the other patient, he started having some symptoms of cough, body aches and low grade fever over the last week. He was scheduled to return to work this next week. His X-ray showed a hint of “infiltrate” which could mean pneumonia. I decided to keep him home and treated him with an antibiotic. He did not want to be retested. Since we were going to keep him off of work anyway, I did not feel that it was necessary at this time.
His wife was feeling pretty cruddy and was in the thick of it with aches, fever, pain in the chest with breathing and a cough. Thankfully her lungs were clear and her vital signs look good. I told her that my suspicion for her was very high in regards to having COVID-19. I wasn’t convinced that testing would be very useful. A positive test would confirm the diagnosis but my “pretest probability” was so high that a negative test would likely be a false negative and it would not change the management approach. I put her on the “positive” list so that she would get called every day. We discussed what symptoms to watch for, about the importance of position changes to keep her lungs aerated, of staying well hydrated and of course, to self-quarantine.
The last individual was young and healthy and had relatively mild symptoms but he did have the distinctive loss of taste. He had no known contacts. His father had traveled to Europe in late February but had no symptoms. He lives at home with younger siblings and both his parents. I felt that it was important to diagnose him definitively from an infection prevention point of view. A positive test will allow a more aggressive message to his family to stay at home and possibly get tested. Other contacts could also be informed.
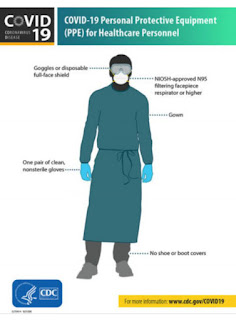
In all, it was an interesting morning. The staff at the clinic were very helpful, very friendly and we worked well as a team. I felt very safe, wearing full PPE with a face shield, N-95 mask, gown, gloves and shoe booties. We cleaned after every patient. The rooms have been fitted to be negative pressure. The clinic is well thought out and well executed. It is the perfect clinic to Make sure that our medical offices are kept safe. They are not set up to do these kind of visits where it would be impossible to take the same precautions. As I finished my shift, I took my shower, changed and came home to do a full afternoon of telemedicine visits on Zoom.
We are urgently considering how to open up our offices to usual patient care. The plan is to keep the respiratory clinic going for quite awhile. This will also help keep the emergency room less crowded and safer for those that need life saving treatment for other conditions such as my patient with the heart attack. Similar thought needs to happen for all of us. How do we adapt to an emerging society? It will still be important to take caution and decide If there are new, safer approaches that will work as well as the older ones. It will be interesting to see how schools, churches and of course businesses open back up. Let’s continue to stay safe and let’s be wise.